The Ultimate Guide to Customer Data Platforms (CDPs)
Customer Data Platforms (CDPs) are among the most hyped and least clearly defined technologies in the modern MarTech stack.
Published on November 25, 2025
In eCommerce, they’ve become nearly indispensable, powering hyper-personalized experiences across every touchpoint. But in healthcare, where privacy risks are higher and the data environment more fragmented, CDPs are often adopted without a clear strategy, avoided entirely due to compliance concerns, or purchased for a use case that doesn’t actually require the investment in a CDP.
Vendors across the MarTech landscape now call themselves CDPs, yet they deliver wildly different functionality. Some are built for real-time orchestration and personalization. Others focus primarily on data collection and warehousing. Still others are just rebranded CRMs claiming CDP capabilities. The label “CDP” has become so stretched that it often obscures more than it clarifies.
This guide is here to clear the fog. It’s built for healthcare marketers, IT leaders, compliance officers, and digital strategists who need to understand:
- What a CDP really is (and what it’s not)
- The core utility vendors use to justify CDP investments
- Where that utility can be found, or built, using other tools
- How to evaluate vendors in a privacy-first, HIPAA-regulated environment
CDPs aren’t “more important” in healthcare than in other industries. But they are riskier to get wrong. When implemented without privacy enforcement, consent awareness, or architectural flexibility, CDPs can become a compliance liability. When implemented well, they can unlock secure, first-party engagement at scale.





What Is a CDP?
At its core, a Customer Data Platform (CDP) is a system that unifies data about individuals from multiple systems, resolves identities across touch points, segments those individuals into audiences, and offers the potential to activate those audiences across digital experiences, marketing and engagement channels.
For healthcare organizations, that might mean:
- Creating a unified profile across EHR, CRM, and digital systems
- Suppressing marketing to unconsented users or current patients
- Orchestrating web personalization and personalized outreach for high-value service lines
But confusion around what qualifies as a CDP is rampant, and in many cases, justified. The term is applied to systems with vastly different architectures and utilities. Many vendors use “CDP” to describe tools that do only a subset of what the term once implied, while other CDPs in the space do much more.
The CDP Promise and Why It’s Fraught in Healthcare
The original promise of the CDP category was both grand and straightforward:
Stitch together anonymous and known data into a single, persistent profile and use it to drive smarter engagement.
That meant linking website behavior to CRM records, identifying users across devices, and triggering real-time personalization based on their actions and attributes.
But in healthcare, this same functionality becomes a liability:
- Linking anonymous sessions to patient records can expose PHI.
- Real-time activation pipelines may bypass consent logic.
- “Personalization” that seems innocuous in ecommerce can appear invasive or noncompliant when tied to a diagnosis, condition or provider interaction.
As a result, vendors targeting healthcare have to evolved. Some focus on audience sync and consent-aware orchestration. Others provide event routers or data pipelines that strip PHI before activation. These are valuable utilities, but they are not always full CDPs. Still, vendors use the term because it’s what buyers are searching for.
This guide aims to bridge the gap between what CDPs were originally meant to do, and what privacy-first organizations actually need today.
A CDP Is Not:
- A CRM: CRMs manage known contacts. CDPs unify behavior across anonymous and known states, often with more dynamic data.
- A Data Warehouse: Warehouses store and analyze data, but doesn’t stitch identities gracefully or drive marketing workflows without extensive modification.
- A Tag Manager: TMS platforms control what gets collected, not how data is unified, segmented, or activated.
- A Consent Management Platform (CMP): CMPs enforce consent, but they don’t unify data or create audiences.
A Healthcare-Grade CDP Must:
- Unify first-party data across platforms in a HIPAA-compliant way
- Resolve identities and link them to consent status
- Segment audiences with privacy-aware filters
- Orchestrate activation without exposing PHI
- Integrate with CMPs, EHRs, CRMs, and outbound channels
- Provide audit-ready logs and suppression capabilities
In essence, a CDP in healthcare must be a privacy-aware data orchestration layer designed to bridge marketing, compliance, and clinical systems without compromising trust.
Why Healthcare May (or May Not) Need a CDP
The conventional wisdom is clear: healthcare organizations need a CDP. Vendors pitch them as the solution to fragmented patient journeys, unstructured data, and rising expectations for personalization. Industry content reinforces the idea that CDPs are a must-have for healthcare marketers.
But here’s the reality: many healthcare organizations don’t need and may not be able to use CDP… at least not yet.
CDPs introduce complexity, cost, and compliance risk. And while their promise is compelling, their utility depends entirely on organizational maturity, internal capabilities, and privacy posture.
So instead of assuming a CDP is needed, let’s ask the better question: what problems are you trying to solve, and is a CDP the right tool for it?
When a CDP May Be Necessary:
You need to unify data across siloed systems
Patient interactions span EHR, CRM, scheduling tools, contact centers, websites, and mobile apps. If you can’t connect those dots, you can’t personalize, suppress, or measure meaningfully.
You want to segment and orchestrate outreach at scale
If you’re trying to run personalized engagement across hundreds of patient segments, while suppressing unconsented individuals and adhering to HIPAA, doing that manually or with disconnected tools isn’t sustainable.
You have the IT and governance maturity to support it
CDPs require strong data governance, clear ownership across marketing and IT, and well-defined integration workflows. Without that foundation, the platform rarely delivers on its promise.
When a CDP May Not Be Necessary:
You’re solving for basic patient acquisition workflows
Many healthcare organizations just need consent-aware analytics and suppression lists synced to advertising platforms. That can be handled with server-side tagging, a CMP, and a warehouse or audience sync tool. No CDP required.
You already unify known data
If your EHR (or CRM) is already the system of record for patient profiles, and it’s integrated with your marketing stack, you may not need a CDP to replicate that function.
Your use cases are few and low-volume
CDPs shine when powering high-volume personalization and segmentation. If you’re only running a handful of campaigns per month, the overhead of a CDP may outweigh the benefit.
You’re not ready to handle PHI in marketing systems
CDPs often require rethinking your compliance model, especially if you’re activating data downstream. If your organization isn’t ready to securely handle PHI or enforce consent across your stack, a CDP could increase risk, not reduce it.
CDP Alternatives in Privacy-First Stacks
For many healthcare teams, the value they seek in a CDP can be found elsewhere:
- Consent-aware analytics and suppression via server-side tagging + CMP
- Audience activation through reverse ETL tools (like Hightouch)
- Data unification through your existing warehouse + ETL processes
- Orchestration via HIPAA-safe marketing automation tools
Bottom line: Healthcare may need a CDP, but only if the organization has the right complexity, readiness, and privacy posture to justify it. Otherwise, the better investment may be in composable tools that offer similar outcomes with less risk. The point isn’t that CDPs are bad. It’s that they’re often overprescribed and underdelivered.
Role in the Healthcare Stack
In the modern healthcare marketing stack, a Customer Data Platform (CDP) or identity resolution layer plays a coordinating role, facilitating data flow between systems rather than dominating it.
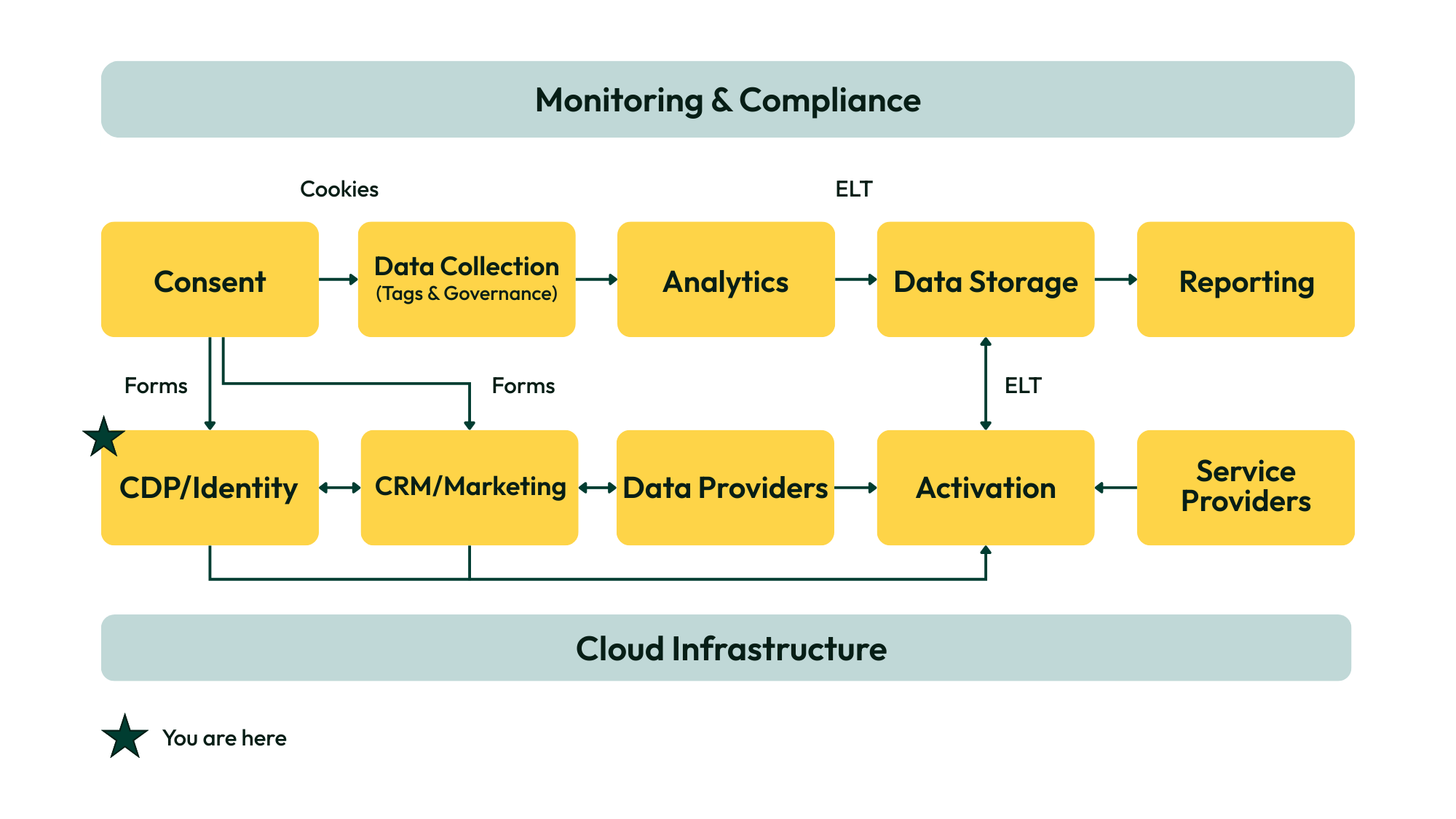
As shown in the diagram above, the CDP/Identity component sits midstream. It connects upstream data inputs like web forms, CRMs, and consent platforms with downstream tools for activation, service delivery, and reporting. This layer ensures that audience segmentation, consent enforcement, and identity stitching happen in a privacy-aware and operationally efficient way.
Functional Positioning in the Stack
- Upstream Inputs: CDPs receive data from consent platforms, CRM/marketing systems, and forms submitted by patients or members. This includes known identifiers, behavioral data (when permitted), and marketing preferences.
- Coordination with Data Providers: The CDP exchanges data with enrichment tools or external platforms to build more complete audience profiles, often filtered or pseudonymized to comply with HIPAA or state regulations.
- Downstream Activation: Audience segments and suppression rules flow from the CDP into activation channels (e.g. email, SMS, call center platforms, and digital advertising) enabling outreach that respects both user preferences and regulatory constraints.
- Integration with Analytics and Storage: In composable stacks, behavioral or activation data may pass through the CDP and be routed into analytics tools or long-term storage for measurement, attribution, and optimization.
Collaborative, Not Centralized
In this architecture, the CDP doesn’t operate as the center of the stack, it acts as a middleware layer that ensures data flows securely, identities are resolved responsibly, and downstream systems only receive data that has been cleared for activation.
The CDP’s effectiveness depends on how well it integrates with consent platforms, cloud infrastructure, and data governance policies, not just how many features it bundles into one product.
Core Capabilities of a Healthcare-Grade CDP
What makes a CDP truly valuable in healthcare is whether the platform can reliably and compliantly support the core capabilities required to unify, protect, and activate first-party data across complex systems and regulated workflows.
Here, we define the seven key capabilities that matter most in HIPAA-compliant environments, along with the business problems they address and how they work in practice.
Data Unification
What it is: Aggregating data from multiple systems (CRM, EHR, web, mobile, call center) into a centralized record structure.
- Goal: Align siloed data around a consistent schema and person/entity
- Common sources: CRM, EHR, call logs, web events, form submissions
- Core activity: Data mapping, normalization, ETL/ELT pipelines
- Output: A unified profile or record
Identity Resolution
What it is: Determining when multiple identifiers (anonymous or known) belong to the same individual.
- Goal: Link sessions, clicks, and offline data to a persistent identity
- Identifiers used: Email, device ID, cookie, phone number, member ID
- Approaches: Deterministic (exact match), probabilistic (signal overlap), or hybrid
- Healthcare nuance: Risky unless consent is explicit; can introduce PHI exposure
Audience Segmentation
What it is: Creating groupings of individuals based on behaviors, attributes, or lifecycle stage for tailored messaging.
- Goal: Define and manage lists or cohorts for outreach and suppression
- Examples: “Medicare-eligible individuals in service area who engaged with orthopedic content but have no scheduled appointments,” “Women 35-50 who researched maternity services, attended a virtual tour, but didn’t schedule a consultation within 30 days.”
- Common filters: Event-based behavior, demographics, CRM attributes, consent status
- Output: Lists or dynamic segments synced to downstream tools
Consent Enforcement
What it is: Ensuring that any data collection or activation aligns with captured user preferences.
- Goal: Prevent marketing actions that violate user consent or HIPAA
- Consent inputs: Web forms, patient portal opt-ins, CMP signals
- Typical behavior: Block/suppress data collection or activation if consent is missing
- Output: Consent flags stored per profile; used for real-time enforcement or segment filtering
Suppression
What it is: Proactively excluding individuals from marketing or outreach based on regulatory, legal, or preference signals.
- Goal: Prevent PHI-sensitive outreach, noncompliant or inefficient audience targeting
- Use cases: Exclude recent patients, minors, or those who revoked consent
- Data sources: Consent systems, CRM tags, EHR signals
- Healthcare nuance: Often more important than activation; critical to avoid fines and brand risk
Activation
What it is: Sending enriched, segmented data to tools that deliver messages or experiences (e.g. email, ads, SMS, call center).
- Goal: Enable campaigns, personalization, and outreach with current, consented data
- Channels: Google Ads, Meta, Salesforce, SMS platforms, email tools
- Methods: Direct integrations, API pushes, Reverse ETL pipelines
- Privacy considerations: Must control what data is sent, where, and under what conditions. Activation arguably creates the greatest risk, related both to data privacy issues and to the potential for poor patient experiences based on personalization that may be perceived as “invasive”
Governance & Audit Logging
What it is: Tracking how data is accessed, processed, shared, and activated, especially in regulated industries.
Healthcare compliance tie-in: Supports HIPAA’s audit requirement and breach defensibility
Goal: Ensure defensibility in audits, reduce unauthorized data exposure
Includes: Access logs, data lineage, change histories, suppression logs
Output: Immutable records of data flow and decisioning
Core Capabilities vs. Alternative Solutions

CDP Vendor Landscape
The CDP category is crowded, inconsistent, and poorly defined. Dozens of platforms use the label, but they differ wildly in architecture, compliance readiness, and actual functionality. To bring clarity, we’ve grouped CDPs into three categories based on how they’re built, and how they serve privacy-first healthcare needs:
- Packaged CDPs – Monolithic, feature-rich platforms with native identity, segmentation, and activation.
- Composable CDPs – Modular tools that integrate around a cloud warehouse.
- Privacy-First CDPs – Purpose-built for HIPAA-regulated environments, emphasizing consent and suppression as core functions.
Within each category, a few vendors stand out—and in the case of Privacy-First CDPs, the category itself is starting to stretch the boundaries of what “CDP” means.
A. Packaged CDPs
Packaged CDPs offer all-in-one solutions for data ingestion, unification, audience segmentation, and multi-channel activation. These platforms appeal to enterprise teams seeking breadth and centralization, and many are already well-entrenched in healthcare and life sciences.
Vendors in this category include:
- Tealium AudienceStream – A strong performer in HIPAA-aligned enterprise CDPs, with real-time event flows and robust integrations.
- Salesforce Health Cloud + CDP – Deep CRM alignment and growing CDP maturity, but often complex to implement across silos.
- Adobe Real-Time CDP – Rich feature set with strong data modeling capabilities; may be heavy for organizations without deep engineering support.
- Treasure Data – A flexible, enterprise-friendly CDP with consent controls and healthcare deployments.
- Redpoint Global – Designed for complex customer journeys; strong segmentation and orchestration engine.
These platforms generally support HIPAA through BAAs and offer various levels of PHI-safe tooling, but often require significant internal infrastructure and governance to implement safely.
B. Composable CDPs
Composable CDPs embrace the warehouse-native model, allowing teams to build their own CDP-like architecture using best-in-class tools. This model favors data maturity, internal engineering support, and modularity over out-of-the-box convenience.
Key players include:
- Hightouch – A leading Reverse ETL tool that allows healthcare teams to sync audiences from Redshift, BigQuery, or Snowflake into activation platforms with consent-aware filtering.
- RudderStack – Offers event streaming, identity resolution, and audience building atop your warehouse. HIPAA support available on higher-tier plans.
- Twilio Segment – Popular for event collection and unification; HIPAA compliance offered only through select plans and enterprise configurations.
Composable CDPs can be highly compliant, but that compliance depends heavily on how the stack is assembled, governed, and maintained.
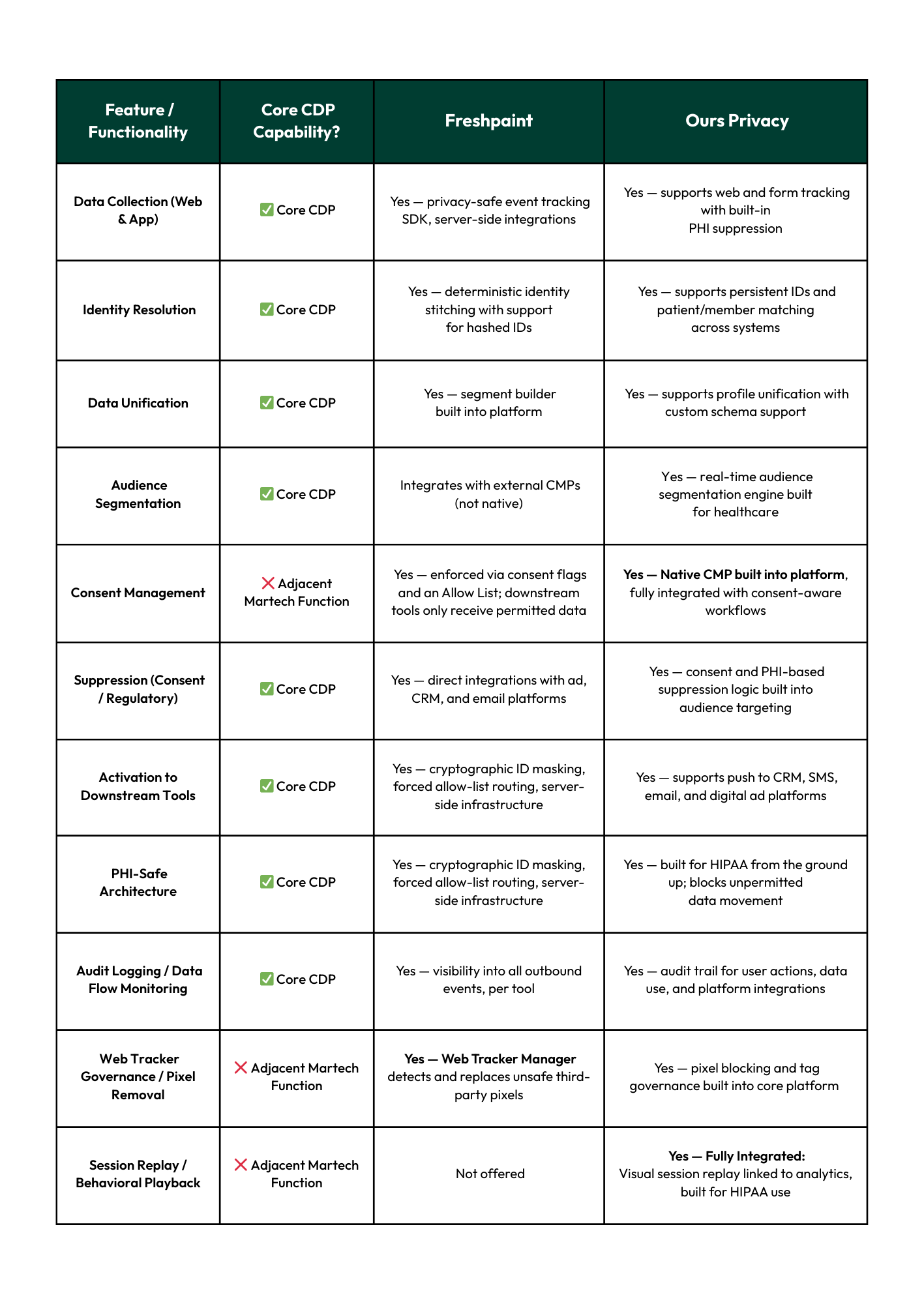
C. Privacy-First CDPs
Privacy-First CDPs are built for HIPAA. These platforms prioritize suppression, consent enforcement, PHI-safe architecture, and governance over feature bloat or marketing automation bells and whistles. They’re leaner, sharper, and often more aligned with the real-world needs of privacy-first organizations.
Freshpaint and Ours Privacy are two leading examples, and while both still use the term “CDP,” their platforms now blur the line between customer data infrastructure and privacy-governed marketing operations.
CDP Vendor Comparison: Freshpaint vs. Ours Privacy
Legend
- ✅ Core CDP Capability: Aligned with traditional definitions (data unification, segmentation, activation, etc.)
- ❌ Adjacent Martech Function: Expands the CDP into new categories (governance, consent, tracker control, UX diagnostics)
Evaluation Framework
To assess HIPAA-ready Customer Data Platforms, we evaluated vendors against five weighted criteria reflecting the demands of privacy-first healthcare organizations.
1. Privacy & Compliance (30%)
This is the non-negotiable category. CDPs serving regulated environments must demonstrate:
- BAA availability (standard or on-demand)
- HIPAA-compliant data architecture, including support for PHI handling and encryption
- Consent enforcement workflows (beyond simple tracking or flagging)
- Fine-grained audit logging and access control
2. Healthcare Fit (25%)
This evaluates how well a platform aligns with healthcare-specific data, workflows, and use cases.
- Presence in healthcare directories and partner ecosystems
- Evidence of adoption in health systems or payer organizations
- Integration support for EHR, CRM, or claims data
- Verticalized messaging, healthcare-specific features, or templates
3. Architecture & Flexibility (20%)
TThis assesses how composable, deployable, and developer-friendly a platform is.
- APIs, SDKs, and engineering extensibility
- Warehouse-native or cloud-agnostic support
- On-premise or private cloud deployment options
- Support for both batch and real-time workflows
4. Core Capabilities (15%)
Beyond privacy scanning, tools should support governance workflows by:This category evaluates how well the platform delivers on the fundamental utility of a CDP:
- Activation and orchestration features
- Identity resolution and profile stitching
- Consent-aware audience segmentation
- Structured/unstructured data unification
5. Usability & Support (10%)
This addresses both the user experience and vendor partnership quality.
- UI/UX accessibility for marketing and data teams
- Quality of API and SDK documentation
- Training, onboarding, and customer success
- Availability of support across technical and non-technical users
Vendor Scorecard for Customer Data Platforms (CDPs)
This table evaluates leading Customer Data Platforms (CDPs) against the needs of privacy-first healthcare organizations. Each vendor is assessed on two key dimensions, compliance utility and marketing enablement, alongside a holistic score that reflects overall performance, flexibility, and fit for HIPAA-regulated environments.
Dual Utility: Compliance vs. Performance
Selecting a CDP in healthcare is about trade-offs. Organizations must weigh two competing imperatives:
- Compliance Utility – How well the platform enforces HIPAA standards, from consent and suppression to PHI-safe architecture and auditability.
- Marketing Enablement – How effectively it supports segmentation, personalization, campaign execution, and performance optimization.
The Dual Utility Framework scores each platform on these two axes (out of 8), then maps them into a quadrant that helps privacy-first organizations evaluate real-world alignment for healthcare marketing.

Future Outlook: CDPs Transition Toward Marketing & Data Platforms
The original promise of a Customer Data Platform (CDP) was simple: unify your customer data, resolve identity, build segments, and activate campaigns. But in privacy-first industries like healthcare, that definition is no longer enough.
CDPs today are under pressure to evolve. As the demands of privacy, compliance, and cross-channel engagement intensify, the platforms that succeed will look less like traditional CDPs and more like fully integrated marketing and data platforms.
From CDP to Privacy-First Engagement Layer
What started as tools for event collection and data unification are now platforms offering:
- Built-in consent management
- Consent-aware segmentation and suppression
- Session replay and behavioral mapping
- Pixel governance and tag enforcement
- Downstream data activation with audit controls
This expansion is strategic. In regulated markets, vendors that can consolidate data, consent, segmentation, and activation into a single, governed platform are better positioned to meet the operational needs of healthcare systems, payers, and privacy-conscious organizations.
Why This Shift Matters in Healthcare
In healthcare, marketing infrastructure must both perform and protect. Teams must ensure that every activation, every segment, and every data flow aligns with consent and regulatory expectations. This requires more than piecing together tools. It requires a platform that is:
- Built for compliance, not retrofitted around it
- Capable of unifying and governing data, not just storing it
- Designed to reduce risk, not just accelerate campaigns
And perhaps just as critically: a platform that replaces multiple vendors, each requiring their own BAA.
This is why the CDPs that will lead the market are consolidating utility across consent, data, and marketing operations, becoming engagement hubs, not just data pipes.
About This Guide
This guide was created through a collaborative process that blended the speed and structure of AI with decades of real-world healthcare marketing experience.
We used AI tools to help us gather, synthesize, and organize foundational information about this category and the vendors included. These tools supported brainstorming, research structuring, and drafting early content sections. We also used AI to transcribe and analyze hours of interviews with our internal experts, vendor partners, and healthcare industry leaders, transforming those conversations into the practical insights shared throughout.
Every section was manually reviewed, edited, and enriched by our team to ensure accuracy, nuance, and relevance to healthcare marketers navigating complex privacy challenges. We refined the structure iteratively, using both AI suggestions and human judgment to create a guide that is clear, credible, and actionable.
While AI helped us work more efficiently, it’s the combination of technology and lived experience that gives this guide its depth and utility.
Created by Wheelhouse DMG
Resources
Legal Disclaimer: The information contained in this communication should not be construed as legal advice on any matter. Wheelhouse DMG is not providing any legal opinions regarding the compliance of any solution with HIPAA or other laws and regulations. Any determination as to whether a particular solution meets applicable compliance requirements is the sole responsibility of the client and should be made after consulting with their own legal counsel.
More Ultimate Guides
Explore our other Ultimate Guides to help you navigate your privacy-compliant MarTech needs.