The Ultimate Guide to Downstream Reporting and Visualization Layers
In healthcare marketing, the final mile of data strategy is often the most overlooked, and the most vulnerable.
Published on October 24, 2025
Downstream reporting and visualization platforms represent that mile: the insight layer where governed data becomes decision-making fuel. For privacy-conscious organizations operating under HIPAA, an expanding patchwork of state privacy laws, and increasingly painful enforcement actions, this layer can either safeguard compliance or unwittingly increase risk.
This guide is built for those who manage that risk: digital marketers, compliance officers, analytics leaders, and IT teams working to deliver insight responsibly. It explores downstream BI through a healthcare-specific lens, mapping the features, risks, and governance strategies that separate compliance gaps from competitive advantage.
What You’ll Find Here and What You Won’t
This guide is not a roundup of “top 10 dashboards.” It does not chase feature checklists or UI comparisons. Instead, it is a vendor-neutral, evidence-backed evaluation of downstream BI platforms in HIPAA-regulated environments. The emphasis is on operational alignment, real-world deployment considerations, and regulatory readiness.





What Is Downstream Reporting & Visualization?
Downstream reporting and visualization platforms are tools used to explore, analyze, and communicate insights from data that has already been collected and stored in governed environments. In healthcare marketing and analytics, these platforms serve as the interface between raw data and actionable insight.
They are sometimes mistaken for analytics tools or customer data platforms (CDPs), but the distinction is important. Downstream BI platforms do not collect behavioral data, process real-time events, or manage patient identities. They do not run tags or tracking scripts. Their sole function is to help teams interpret structured datasets that have already been passed through upstream governance, transformation, and de-identification pipelines.
At a technical level, these platforms sit atop cloud data warehouses like Snowflake, BigQuery, and Redshift. They connect to compliant datasets, apply semantic models, and allow users to filter, segment, visualize, and report on that data without exposing sensitive information.
From a compliance perspective, this layer must be treated with the same rigor as data ingestion and storage. If a dashboard reveals too much detail, allows unrestricted exports, or is embedded in a public-facing portal without safeguards, it can transform de-identified data into a regulatory risk.
A properly implemented downstream platform provides value without vulnerability. It reflects governed data, respects access controls, and allows insight to travel only as far as policy permits. It enables healthcare marketers and analysts to ask better questions of their data, without opening doors that compliance teams would rather keep closed.
This governance-first view is what shaped our approach to Compass, our HIPAA-compliant data warehouse. It’s designed to solve the problems outlined above: connecting disparate data sources using normalized data from a variety of channels, providing consistent naming conventions, and ensuring that downstream reporting reflects reality. The goal is to make sure what teams see is both actionable and safe, within a HIPAA-compliant infrastructure that doesn’t force compromises between insight and governance.
Why Downstream BI Matters in Healthcare
Downstream reporting platforms typically operate in the background. Until they don’t. These tools are the lens through which executive teams, compliance leaders, and marketers view their data. And when that lens distorts, omits, or exposes too much, the consequences ripple across legal, operational, and reputational lines.
This is especially critical under HIPAA’s “minimum necessary” standard. Visualizations must reflect not just what data is available, but what is appropriate to share.
Many teams still rely on Excel exports or reporting directly from analytics platforms. These approaches lack role-based access control, audit logging, or suppression of unconsented records. Even sophisticated tools like Tableau or Power BI can become liabilities if deployed in ways that allow unrestricted access or cloud-hosted extraction without proper configuration.
Beyond risk, there is also opportunity. When deployed with intention, downstream BI enables privacy-safe analysis across marketing performance, operational metrics, and patient experience. It becomes the translation layer between governed data and actionable strategy, as long as the data is clean, the platform is configured, and the users are trained.
Role in the Healthcare Stack
The diagram below maps this architecture from left to right, showing how consent signals, identity stitching, analytics, and activation tools interact within a compliant cloud environment. Downstream BI platforms appear at the far right signaling their position as the last stop before insights are consumed and shared across the organization.
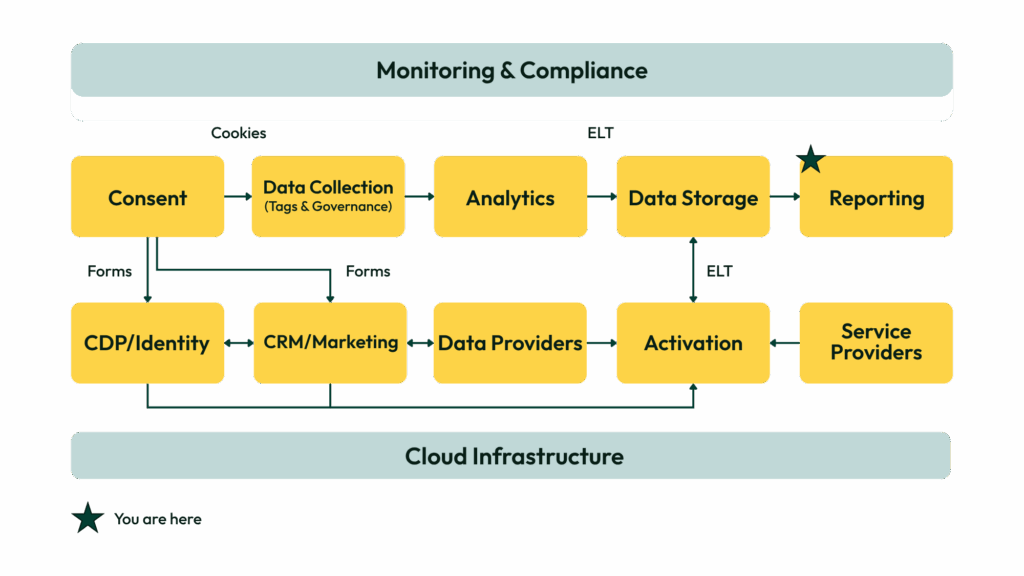
This layer depends on everything upstream: accurate tagging, consistent event naming, structured identifiers, and well-managed warehouse pipelines. But it also feeds forward. Reporting influences what stakeholders believe is working, which campaigns get funded, and what patient journeys are prioritized. It becomes a key lever for strategy and storytelling, and a potential fault line for compliance.
If role-based access controls aren’t configured, dashboards can leak sensitive data. If export permissions are too open, compliance teams lose traceability. If visualizations are disconnected from upstream governance logic, insights drift from reality.
The downstream BI layer must be configured to reflect truth, respect limits, and invite trust from both analysts and decision-makers. It is where the privacy posture of your stack becomes visible, to the people who make choices with it every day.
Core Capabilities
Downstream BI platforms may look interchangeable at first glance. Most offer charts, dashboards, and export tools. But in regulated healthcare environments, the difference between a decent platform and a deployment-ready one comes down to specific features that support secure insight generation without creating compliance gaps.
A strong platform must connect securely to governed environments, respect user roles, suppress sensitive data when required, and enable auditability without manual intervention. Below are the foundational capabilities we consider essential when evaluating downstream BI tools for HIPAA-aligned use.
Secure Data Connectivity
A modern BI tool must offer direct integration with governed data stores such as Snowflake, Redshift, or BigQuery. These connections must support encrypted data transfer, private subnet configurations, and metadata logging to prevent unauthorized access or backchannel extraction.
Role-Based Access Control (RBAC)
Granular permissioning is non-negotiable. Platforms should support multiple user roles with tightly scoped access — by dashboard, dataset, field, or row. This includes the ability to restrict PHI exposure based on user function or department, and to prevent unnecessary access to high-risk segments.
De-Identified and Aggregate Reporting
Dashboards must be designed to surface trends, not individuals. Strong platforms support aggregation thresholds, cohort suppression, and dynamic redaction to ensure outputs remain compliant even as data updates. This is particularly important for tools embedded outside the firewall or shared with partners.
Audit Logging and Access Monitoring
BI platforms must log all access events, user interactions, and export activities. These logs should be immutable and retrievable for compliance reviews. Alerting on unusual access or data usage patterns adds a layer of operational security and audit readiness.
Semantic Layer and Metrics Modeling
Platforms should support the creation of governed metrics layers that standardize definitions across users and teams. This prevents conflicting interpretations of KPIs and ensures consistency between visualizations and strategic narratives.
Embedded and External Sharing Controls
For teams that need to embed dashboards in portals or share links externally, the platform must offer secure embedding protocols, tokenized access, and view-level permissions. Without these, even well-governed data can leak through unsecured visual interfaces.
AI-Enabled Exploration
Leading platforms now offer natural language querying, anomaly detection, and scenario modeling powered by AI. These features reduce dependence on data analysts and allow marketing, strategy, and operations teams to ask deeper questions directly in the interface — without writing SQL or building custom dashboards. However, care should be taken to ensure such implementations use either local LLMs (ensuring no data sharing) or AI capabilities designed and deployed specifically for highly regulated industries.
Vendor Landscape
The downstream BI market is mature, but fragmented. Most platforms were not built with HIPAA in mind, and few offer turnkey support for PHI-safe deployments. This creates a wide gulf between tools that can be deployed out of the box and those that require workarounds, governance layers, or architectural compromises to meet compliance requirements.
To help teams navigate this complexity, we categorize BI platforms into two primary tiers based on their ability to support HIPAA-regulated use cases.
Tier 1: HIPAA-Native Platforms
These tools offer out-of-the-box support for HIPAA compliance when deployed within eligible infrastructure and configured correctly. They provide audit logging, access controls, encryption, and are willing to sign BAAs. Most also support deployment models that restrict PHI exposure and enable robust governance.
Power BI (Azure-native, HIPAA-ready with BAA)
Supports RBAC, encryption, audit trails, and private cloud or on-prem hosting. Integration with Microsoft 365 makes it attractive for healthcare enterprises already on Azure.
Amazon QuickSight (HIPAA-ready under AWS BAA)
Serverless BI platform tightly integrated with Redshift and S3. Offers AI features for natural querying and anomaly detection. Composable architecture makes it flexible for teams using Compass or similar HIPAA-governed data environments. Quick Sight is now part of a broader AI-driven offering from Amazon called Quick Suite, which gives it far more utility as an analysis tool.
Tableau (HIPAA-eligible when self-hosted or via Tableau Cloud with healthcare deployment)
Popular among enterprise users. Cloud version now offers HIPAA-supporting deployment models, but most compliance-conscious teams still prefer self-hosting.
Sisense (Multi-cloud or on-prem)
Offers PHI-safe embedded analytics, RBAC, and white-labeled dashboards. HIPAA support available via secure deployment configurations on AWS or Azure.
Tier 2: Compliant-via-Pipeline Tools
These platforms are not inherently HIPAA-compliant, but can be used safely when layered atop de-identified data and paired with strict access controls. They are often easier to adopt but carry more risk without supporting infrastructure.
Looker Studio (Formerly Google Data Studio)
Free and accessible, but lacks support for RBAC or export restrictions. Not covered under Google’s BAA. Defaults to permissive sharing and requires caution in regulated environments.
Metabase
Open-source BI tool that can be hosted privately. Lacks HIPAA-native features but can be deployed safely within governed infrastructure and paired with suppression rules.
Domo
Cloud-first tool with strong visualization features. HIPAA compatibility depends on deployment model and surrounding governance. Often used in marketing teams for campaign reporting.
ThoughtSpot
AI-driven interface built for natural language querying. Can support HIPAA-compliant use when deployed in private cloud or through federated access to de-identified data sources.
Evaluation Framework
To assess HIPAA-ready Downstream Reporting & Visualization Platforms, we evaluate vendors against five weighted criteria:
1. Privacy & Compliance (30%)
This is the non-negotiable category. Platforms must demonstrate:
- HIPAA-compliant deployment options (e.g., BAA availability, private cloud, on-prem hosting)
- Secure data connections to governed warehouses (Snowflake, Redshift, BigQuery)
- Encryption at rest and in transit
- Support for audit logging, user access tracking, and role-based controls
- Data suppression or de-identification workflows to prevent PHI exposure
2. Reporting Functionality & Data Modeling (25%)
- Interactive dashboards with filtering, drill-downs, and ad hoc exploration
- Custom metrics and semantic layer capabilities for standardized reporting
- Report scheduling and export automation
- Ability to adapt visualizations for both technical and non-technical users
3. Healthcare Fit & Use Cases (20%)
- Adoption in health systems, provider networks, or payer organizations
- Support for campaign performance tracking, patient journey views, or operational dashboards
- Industry-specific case studies or messaging for healthcare marketing and compliance teams
4. Governance, Access Control & Sharing (15%)
- Role-based access down to the field or row level
- Permissions by workspace, dashboard, or user group
- Controls for secure embedding, download restrictions, and view-only sharing
- Logging of dashboard changes, exports, and view activity
5. Deployment Flexibility & Integration (10%)
- Availability of cloud, hybrid, or self-hosted models
- Seamless integration with cloud environments like AWS, Azure, and GCP
- Support for programmatic access, APIs, or SDKs for embedding and automation
Vendor Scoring
To help teams select the right downstream BI platform, we’ve translated the evaluation rubric into a scorecard that reflects both compliance strength and insight delivery potential. This table summarizes how each downstream BI platform performs across privacy, governance, reporting functionality, and healthcare usability dimensions.
Among the most widely used tools — Amazon QuickSight, Power BI, and Tableau — each offers a different balance of enforceability, governance features, and usability for healthcare teams.
Amazon QuickSight
QuickSight received the highest overall score based on its HIPAA-eligible deployment model, native AWS integration, and modern analytics features. It scored strongly across all five evaluation dimensions, especially in Privacy & Compliance Controls and Deployment Flexibility.
QuickSight’s Compliance Utility score reflects secure architecture (BAA, encryption, RBAC, audit logging) and clear deployment pathways within governed AWS environments. Performance Utility is equally strong thanks to natural language querying, anomaly detection, and seamless integration with Redshift and S3, all without requiring advanced configuration or data engineering overhead.
Power BI (Microsoft)
Power BI scored just below QuickSight overall. It matches or exceeds many compliance expectations under Azure, with native support for RBAC, encryption, and detailed audit logs. It also integrates tightly with other Microsoft platforms such as Dynamics and Synapse.
Its Compliance Utility score is high, particularly for teams already standardized on Microsoft cloud infrastructure. Performance Utility is also solid, although the platform is more analyst-oriented and can be complex for non-technical users to navigate. Governance features are robust, but visual customization and AI capabilities are more limited compared to newer platforms.
Tableau (Salesforce)
Tableau remains widely adopted in healthcare, particularly among organizations with established data teams or embedded Salesforce environments. It performed well in Reporting Functionality and Healthcare Fit, but overall score was lowered by deployment complexity and limited native compliance support in Tableau Cloud.
Its Compliance Utility score is strong when self-hosted or deployed within a HIPAA-compliant cloud configuration. However, Tableau Cloud requires more diligence and configuration to meet minimum necessary standards. Its visual interface is highly flexible, but the platform lacks built-in AI features and natural language querying that now define higher-performing tools in this space.
Dual Utility: Compliance vs. Performance
In healthcare, BI platforms are often selected based on usability or visualization features. These criteria are important, but on their own they don’t reflect the operational risk tied to how data is accessed and shared. In regulated environments, a downstream reporting tool must enable insight without exposing sensitive data or violating privacy rules.
The Dual Utility Framework provides a way to assess each platform through two critical lenses — whether it enforces privacy safeguards, and whether it enables meaningful use across teams.
When deployed correctly, HIPAA-aligned BI platforms support the following:
Compliance Utility
- HIPAA-eligible deployment options with signed BAA
- Secure integrations with governed data stores like Redshift, BigQuery, or Snowflake
- Role-based access controls and row-level suppression to protect sensitive cohorts
- Audit logging, export monitoring, and traceability for all users and dashboards
Performance Utility
- Natural language querying and AI features to reduce analyst bottlenecks
- Interfaces that support marketers, compliance leaders, analysts, and operations staff
- Seamless data flow from governed warehouses into de-identified reports or dashboards
- Automated delivery of insights, scheduled exports, and decision-ready visualizations
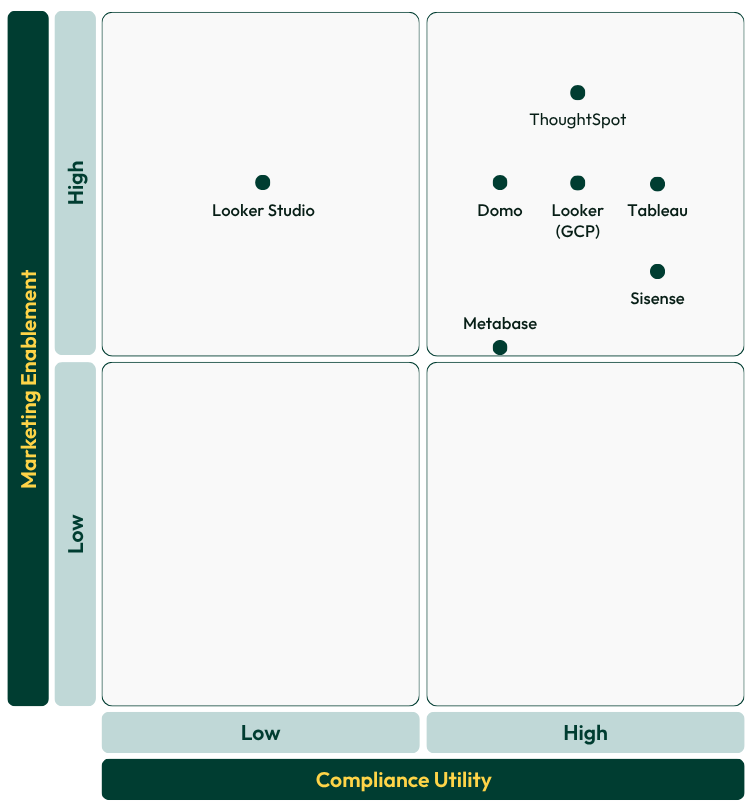
Visualizing Platform Positioning: Compliance vs. Performance
The Dual Utility Matrix maps downstream BI platforms along two dimensions that matter in healthcare environments:
- Compliance Utility reflects the platform’s ability to enforce privacy, restrict access, and maintain auditability under HIPAA and related frameworks.
- Performance Utility reflects how well the platform supports use across teams, connects with upstream systems, and delivers strategic insight.
Each platform falls into one of four quadrants based on these dimensions:
Top-right (High Compliance, High Performance)
QuickSight and Power BI score strongly on both axes. These platforms support secure deployment and structured access while offering automation, advanced visualization, and AI-powered exploration.
Top-left (High Compliance, Moderate Performance)
Tools like Tableau and Sisense provide the infrastructure and governance needed for PHI-adjacent use, but they may limit flexibility or require deeper configuration to support business users at scale.
Bottom-right (Moderate Compliance, High Performance)
ThoughtSpot and Domo are strong in usability and insight generation. They can serve healthcare teams well when layered on de-identified datasets, but require clear governance policies to avoid risk.
Bottom-left (Moderate Compliance, Moderate Performance)
Looker Studio and Metabase lack native support for HIPAA or secure access control. These tools are best used for non-PHI datasets or secondary reporting layers where risk is already mitigated.
Implementation Guidance
Deploying a downstream BI platform in a healthcare organization involves more than provisioning access or standing up dashboards. Successful implementation requires alignment across data governance, compliance, marketing operations, and IT, and attention to the specific risks that emerge when insight becomes accessible to broader teams.
A platform may offer HIPAA-compliant features, but those features only matter when they’re configured, maintained, and enforced. Implementation is where compliance posture turns into real-world behavior.
Key Considerations for Deployment
1. Choose the Right Hosting Model
Ensure the platform is deployed within a HIPAA-eligible cloud environment. For tools like Tableau or Metabase, this may mean self-hosting. For others, it involves scoping deployment within AWS, Azure, or GCP and confirming that a signed BAA is in place. Review your provider’s HIPAA documentation to understand whether security controls are enabled by default or require manual configuration.
2. Connect to Governed, Modeled Data
Only connect your BI tool to datasets that have already been de-identified, permissioned, or structured to avoid PHI exposure. Avoid connecting dashboards directly to raw data sources unless they are secured through warehouse-level policies and suppression logic. The reporting layer should reflect only what’s safe to share.
3. Implement Role-Based Access Control (RBAC)
Define access roles that reflect job functions and data needs. Grant the least amount of access necessary for each user or team. Configure access at the dataset, dashboard, and field level. Ensure that marketing users do not have access to identifiers, sensitive dimensions, or small cohort slices that increase re-identification risk.
4. Suppress or Exclude Risky Data Segments
Use filters, thresholds, and dynamic logic to prevent dashboards from rendering data for users who haven’t consented, or for cohorts below a safe aggregation count. Set default filters to exclude non-consented sessions or users wherever applicable.
5. Enable and Monitor Audit Logging
Logging should cover who accessed which dashboard, when they accessed it, and what was exported or shared. Logs should be stored in an immutable location, accessible to compliance or security teams during audits or investigations. Platforms that offer native logging should be preferred over those that rely on external workarounds.
6. Document Governance Policies
Define and document who owns each dashboard, how often it’s reviewed, and what data sources it pulls from. Create a process for reviewing dashboards for compliance with suppression rules and user access controls on a recurring basis.
7. Train Internal Stakeholders
Ensure that every user understands what the platform is, and is not, designed to show. Train marketers and analysts on the limits of de-identified data, export policies, and what to do if they encounter unexpected data in a dashboard.
Future Outlook
The role of downstream BI in healthcare is evolving. What once served as a back-office analytics tool now sits at the center of decision-making across marketing, operations, and compliance. As that role expands, the expectations placed on these platforms are rising, both in terms of technical capability and regulatory responsibility.
AI is already reshaping how teams interact with dashboards. Natural language queries, automated trend detection, and AI-generated recommendations are reducing friction for business users. This can improve adoption and accelerate insight, but it also introduces new risk. If AI tools operate on datasets that include sensitive information or are trained on data without appropriate boundaries, the speed of insight can become a liability.
At the same time, the regulatory bar continues to rise. HIPAA is no longer the only standard teams need to meet. State privacy laws, FTC guidance, and upcoming federal frameworks all point toward a future where accountability extends to how data is interpreted and shared, not just how it is collected or stored.
Healthcare organizations will need to treat downstream BI not as a reporting tool, but as a governed interface. It must reflect institutional privacy posture, carry forward suppression logic, and restrict what users can see based on evolving rules and consents. That governance will need to extend into embedded dashboards, scheduled exports, and any output generated by AI assistants.
In the near future, downstream reporting platforms will likely be evaluated on how well they support:
- AI-powered insight without compromising de-identification
- Consent-aware filtering and dynamic access control
- Integration with clean rooms, suppression layers, and privacy engines
- Interoperability across compliance teams, marketing departments, and data governance stakeholders
About This Guide
This guide was created through a collaborative process that blended the speed and structure of AI with decades of real-world healthcare marketing experience.
We used AI tools to help us gather, synthesize, and organize foundational information about this category and the vendors included. These tools supported brainstorming, research structuring, and drafting early content sections. We also used AI to transcribe and analyze hours of interviews with our internal experts, vendor partners, and healthcare industry leaders, transforming those conversations into the practical insights shared throughout.
Every section was manually reviewed, edited, and enriched by our team to ensure accuracy, nuance, and relevance to healthcare marketers navigating complex privacy challenges. We refined the structure iteratively, using both AI suggestions and human judgment to create a guide that is clear, credible, and actionable.
While AI helped us work more efficiently, it’s the combination of technology and lived experience that gives this guide its depth and utility.
Created by Wheelhouse DMG
Resources
Legal Disclaimer: The information contained in this communication should not be construed as legal advice on any matter. Wheelhouse DMG is not providing any legal opinions regarding the compliance of any solution with HIPAA or other laws and regulations. Any determination as to whether a particular solution meets applicable compliance requirements is the sole responsibility of the client and should be made after consulting with their own legal counsel.
More Ultimate Guides
Explore our other Ultimate Guides to help you navigate your privacy-compliant MarTech needs.